Did you know?
- A concussion is a mild traumatic brain injury (mTBI) and can be sustained from impact to ANY part of the body.
- Concussion prevention strategies (ie. helmets and mouth guards) can reduce the number and severity of concussions in many sports.
- Mild concussion symptoms often resolve within 10-14 days if properly managed- seek guidance! Just because your symptoms are “minor”, doesn’t mean they will resolve without purposeful intervention!
- Complete rest is only appropriate during the acute phases of concussion (first 24-48 hours), after which, symptom-guided activity/exercise should be re-introduced.
- There are many (5+) different causes for your concussion-related headaches. *Headaches can also arise from medication-overuse (ie. acetaminophen>15 days/month)*
- There are even more (10+) different causes for your concussion-related dizziness- one of the most common post-concussion symptoms.
- Clinical diagnosis and thus, treatment planning requires a thorough, and multi-faceted approach, often involving multiple liaising practitioners.
- Concussion cannot be diagnosed via imaging because symptoms arise from a disruption of neurological processes vs. structural damage.
- Previous concussion history (in particular, when poorly managed) is one of the largest predictors of persistent (>3months) concussion symptoms!
The below image helps to summarize the multi-faceted nature of concussion symptoms.
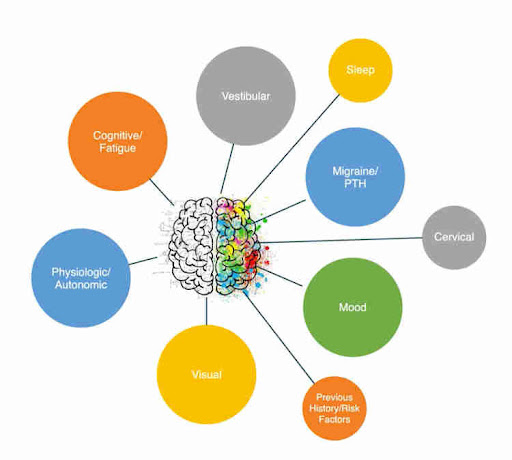
Image provided by Shift Concussion Management Level 2 course material.
So what is involved in concussion rehabilitation, you ask? The short, annoying answer is, it depends (on your presentation, your history, your work/sport goals). I am going to attempt to concisely break down the long answer, which may involve any/all of the following:
Cardiovascular exercise:
Studies show that concussion symptoms can be associated with altered cerebrovascular regulation (control mechanisms of blood flow to your brain). This phenomenon is termed autonomic dysregulation- and should be evaluated using a graded exercise test as soon as possible. If this is in fact a driver of your symptoms, a symptom-guided, progressive exercise program should be commenced to normalize your nervous system’s response to exertion.
Cervical rehabilitation:

Your upper cervical spine (neck) plays a vital role in coordinating head and neck movements in relation to the visual system, as well as providing accurate perceptual information and reactive control relating to your head and neck’s orientation in space. Increased cervical muscle tone (tightness), causing headaches, can arise from the traumatic impact itself, as well as in a protective response to your symptoms (dizziness, disequilibrium). Treatment for all of the above may involve manual therapy, IMS, and corrective exercise.
Vestibular/ocular rehabilitation:
Your vestibular system is highly interconnected with your oculomotor (visual) system and cervical spine (as discussed above). Altogether, they provide us with a clear, accurate, dynamic and adaptable perception of our surroundings. In 60% of concussion cases, this typically well-oiled machine is impaired in one way or another, which may lead to one or more of the following symptoms:
- Dizziness, disequilibrium, nausea, motion sickness, imbalance/gait abnormalities, blurred/double/shaky vision, fogginess, fatigue, cognitive challenges, light sensitivity, difficulty with visual scanning/tracking (reading, driving), discomfort in busy environments (grocery stores), and headaches (eye strain).
Due to the complexity of possible impairments, treatment is complex, multi-faceted and may involve multiple practitioners. Also due to the complexity and nature of impairments, this is often the most commonly mismanaged source of symptoms.
Cognitive/social/work:
Other common predictors of post-concussion recovery timeline include depression/anxiety, pre-existing cognitive challenges/learning disability, female gender, migraine history, sleep challenges. In cases involving any/all of the above risk factors, involvement of an occupational therapist (OT), psychologist and/or counsellor can be an integral piece of the recovery puzzle. Symptom management and successful return to normal activity may involve cognitive behavioural therapy, energy management/task prioritization, coping strategies, breathing techniques, etc.
Sport:

Evidence-based guidelines for concussion management in high level athletes differs from that of non-athletes. For example, athletes have been shown to tolerate and positively respond to exercise at a higher % of their heart rate symptom threshold. Rehabilitation goals relating to work and activities of daily living should precede those of return to sport. Safe re-introduction of strength and conditioning should be carefully re-introduced after resolution of autonomic dysregulation and in collaboration with higher level vestibular/ocular exercises.
Remember, your concussion presentation is unique and cannot follow the same rehabilitation pathway as that of your previous concussion, or your colleague/friend/teammate!
References available upon request.
Written by
Jenny Lehmann
one of our great Physiotherapist
Original post


